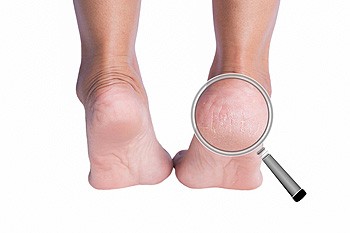
Foot care is especially important for seniors who are more apt to experience falling and mobility issues than those who are younger. Feet change as one ages. Normal changes that happen to feet with age include thick cartilage and fat pads on the soles becoming thinner, the skin and connective tissue becoming fragile and thin, toenails becoming more brittle and prone to fungal infection, and the ligaments holding bones together stretch making feet wider and flatter. Because it is hard for seniors to lean down and bend over, they often neglect foot care. Health conditions can show up aging feet, such as persistent swelling of legs and feet signifying cardiovascular, lymphatic, or kidney disease. Other challenges are cold feet from poor circulation resulting from heart disease, high blood pressure, or nerve damage from diabetes, and foot bone pain from osteoporosis. Seniors are also at risk for bunions, blisters, ingrown toenails, and hammertoes as well. If you are a senior, it is suggested that you visit a podiatrist who can evaluate your feet and provide guidance on how to best take care of them for the highest degree of comfort.
Proper foot care is something many older adults forget to consider. If you have any concerns about your feet and ankles, contact one of our podiatrists from Biebel & DeCotiis Podiatry Associates. Our doctors can provide the care you need to keep you pain-free and on your feet.
The Elderly and Their Feet
As we age we start to notice many changes in our body, but the elder population may not notice them right away. Medical conditions may prevent the elderly to take notice of their foot health right away. Poor vision is a lead contributor to not taking action for the elderly.
Common Conditions
- Neuropathy – can reduce feeling in the feet and can hide many life-threatening medical conditions.
- Reduced flexibility – prevents the ability of proper toenail trimming, and foot cleaning. If left untreated, it may lead to further medical issues.
- Foot sores – amongst the older population can be serious before they are discovered. Some of the problematic conditions they may face are:
- Gouging toenails affecting nearby toe
- Shoes that don’t fit properly
- Pressure sores
- Loss of circulation in legs & feet
- Edema & swelling of feet and ankles
Susceptible Infections
Diabetes and poor circulation can cause general loss of sensitivity over the years, turning a simple cut into a serious issue.
If you have any questions please feel free to contact one of our offices located in Holmdel and Middletown, NJ . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.