Connect With Us
Blog
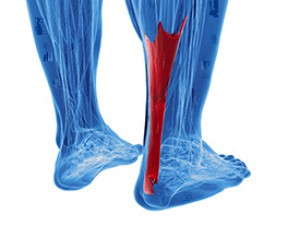
The Achilles tendon is the strongest tendon in the human body. Its purpose is to connect the lower leg muscles and calf to the heel of the foot. This tendon is responsible for facilitating all types of movement, like walking and running. This tendon provides an enormous amount of mobility for the body. Any injuries inflicted to this tissue should be immediately brought up with a physician to prevent further damage.
The most common injuries that can trouble the Achilles tendon are tendon ruptures and Achilles tendinitis. Achilles tendinitis is the milder of the two injuries. It can be recognized by the following symptoms: inflammation, dull-to-severe pain, increased blood flow to the tendon, thickening of the tendon, and slower movement time. Tendinitis can be treated via several methods and is often diagnosed by an MRI.
An Achilles tendon rupture is trickier to heal, and is by far the most painful injury. It is caused by the tendon ripping or completely snapping. The results are immediate and absolutely devastating, and will render the patient immobile. If a rupture or tear occurs, operative and non-operative methods are available. Once the treatment begins, depending on the severity of the injury, recovery time for these types of issues can take up to a year.
Simple preventative measures can be taken as a means to avoid both injuries. Prior to any movement, taking a few minutes to stretch out the tendon is a great way to stimulate the tissue. Calf raises, squats, leg curls, leg extensions, leg raises, lunges, and leg presses are all suggested ways to help strengthen the lower legs and promote Achilles tendon health.
Many problems arise among athletes and people who overexert themselves while exercising. Problems can also happen among those who do not warm up properly before beginning an activity. Proper, comfortable shoes that fit correctly can also decrease tendon injuries. Some professionals also suggest that when exercising, you should make sure that the floor you are on is cushioned or has a mat. This will relieve pressure on the heels. A healthy diet will also increase tendon health.
It is very important to seek out a podiatrist if you believe you have an injury in the Achilles region. Further damage could result in severe complications that would make being mobile difficult, if not impossible.
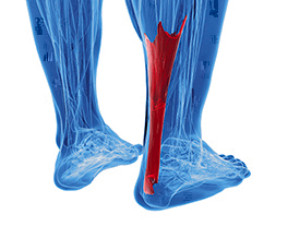 When your Achilles tendon, which connects the calf muscles to the heel bone, is overused, the area may become inflamed. This is a condition known as insertional Achilles tendonitis. In active adults, it is often caused by repetitive use through running or jumping. Symptoms include a sharp pain in the back of the heel, or in some cases, a dull ache. The area will be tender to the touch, and redness and swelling often develops. The first thing you can do is to rest the foot and apply ice to reduce pain and swelling. Try not to rub or poke the area. Non-steroidal anti-inflammatory medication, which can be prescribed by a podiatrist, may help to reduce the inflammation. Once inflammation in the area has diminished there are a number of exercises you can do to strengthen the calf muscles. This will be key to keep from developing chronic tendonitis of the tendon. It is a good idea to visit a podiatrist for a full diagnosis, treatment options, and a list of exercises you can do.
When your Achilles tendon, which connects the calf muscles to the heel bone, is overused, the area may become inflamed. This is a condition known as insertional Achilles tendonitis. In active adults, it is often caused by repetitive use through running or jumping. Symptoms include a sharp pain in the back of the heel, or in some cases, a dull ache. The area will be tender to the touch, and redness and swelling often develops. The first thing you can do is to rest the foot and apply ice to reduce pain and swelling. Try not to rub or poke the area. Non-steroidal anti-inflammatory medication, which can be prescribed by a podiatrist, may help to reduce the inflammation. Once inflammation in the area has diminished there are a number of exercises you can do to strengthen the calf muscles. This will be key to keep from developing chronic tendonitis of the tendon. It is a good idea to visit a podiatrist for a full diagnosis, treatment options, and a list of exercises you can do.
Achilles tendon injuries need immediate attention to avoid future complications. If you have any concerns, contact one of our podiatrists of Biebel & DeCotiis Podiatry Associates. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Is the Achilles Tendon?
The Achilles tendon is a tendon that connects the lower leg muscles and calf to the heel of the foot. It is the strongest tendon in the human body and is essential for making movement possible. Because this tendon is such an integral part of the body, any injuries to it can create immense difficulties and should immediately be presented to a doctor.
What Are the Symptoms of an Achilles Tendon Injury?
There are various types of injuries that can affect the Achilles tendon. The two most common injuries are Achilles tendinitis and ruptures of the tendon.
Achilles Tendinitis Symptoms
- Inflammation
- Dull to severe pain
- Increased blood flow to the tendon
- Thickening of the tendon
Rupture Symptoms
- Extreme pain and swelling in the foot
- Total immobility
Treatment and Prevention
Achilles tendon injuries are diagnosed by a thorough physical evaluation, which can include an MRI. Treatment involves rest, physical therapy, and in some cases, surgery. However, various preventative measures can be taken to avoid these injuries, such as:
- Thorough stretching of the tendon before and after exercise
- Strengthening exercises like calf raises, squats, leg curls, leg extensions, leg raises, lunges, and leg presses
If you have any questions please feel free to contact one of our offices located in Holmdel and Middletown, NJ . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
Although ankle sprains may not be as serious as a broken ankle, they should be given immediate attention and care. An ankle sprain can lead to a significant amount of pain, as well as limited mobility. They are often characterized by the swelling and discoloration of the skin. This occurs when the ligaments are stretched beyond their limits.
The simple act of walking can sometimes cause a sprain, which makes ankle sprains a very common injury that can happen to anyone. They occur when the ankle twists in an awkward way or rolls over itself, causing a pop or snap in the tendons around the ankle. Some people are more at risk than others. These include athletes who continually push their bodies to the limits and also people who have previously suffered accidents to the feet, ankles, or lower legs.
Most of the time, an ankle sprain is not severe enough for hospital attention. There are many at-home treatment options available, including propping the leg up above your head to reduce blood flow and inflammation, applying ice packs to the affected area as needed, taking over-the-counter pain relievers and anti-inflammatory medication, using an ACE bandage to wrap and support the injured ankle, and most importantly, remaining off your feet until the ankle has fully healed.
Despite this, an ankle sprain can turn into a severe injury that might require hospitalization. If the ankle ligaments or muscles are damaged from a tear or rip, that is one sign that the sprain is severe enough for hospital attention and possibly for surgery. Even after the surgery, the recovery process can be long. You may need to have rehabilitation sessions administered by your podiatrist to get your ankle back to full health.
The severity of your sprain might become apparent if you are unable to stand or walk, consistent pain occurs over a prolonged period of time, swelling is much more severe than initially present, or if you start to experience tingling or numbness. These signs may indicate that your ankle sprain might actually be a broken ankle, an injury that requires immediate medical attention.
Although they are not completely avoidable, ankle sprains can be curbed with some preventative treatment measures. These include wearing appropriate-fitting shoes that not only provide a comfortable fit, but also ankle support. It is also recommended to stretch before doing any kind of physical activity, as this will help lower your body’s chance for an injury.
Sprained ankles are a common injury, particularly among athletes. They cause symptoms such as pain, swelling, a limited range of motion, and difficulty walking or bearing weight on the affected ankle. Ankle sprains occur when one or more of the ligaments in the ankle are overstretched or torn. There are two main types of ankle sprains – high ankle sprains and lateral ankle sprains. While their symptoms are similar, treatments can vary. Because of this, getting a proper diagnosis is very important. A podiatrist can diagnose the type of ankle sprain that you have by completing a thorough physical examination of the ankle. Imaging tests may also be used. If you suspect that you may have sprained your ankle, it is strongly suggested that you seek the care of a podiatrist.
Ankle sprains are common but need immediate attention. If you need your feet checked, contact one of our podiatrists from Biebel & DeCotiis Podiatry Associates. Our doctors can provide the care you need to keep you pain-free and on your feet.
How Does an Ankle Sprain Occur?
Ankle sprains take place when the ligaments in your ankle are torn or stretched beyond their limits. There are multiple ways that the ankle can become injured, including twisting or rolling over onto your ankle, putting undue stress on it, or causing trauma to the ankle itself.
What Are the Symptoms?
- Mild to moderate bruising
- Limited mobility
- Swelling
- Discoloration of the skin (depending on severity)
Preventing a Sprain
- Wearing appropriate shoes for the occasion
- Stretching before exercises and sports
- Knowing your limits
Treatment of a Sprain
Treatment of a sprain depends on the severity. Many times, people are told to rest and remain off their feet completely, while others are given an air cast. If the sprain is very severe, surgery may be required.
If you have suffered an ankle sprain previously, you may want to consider additional support such as a brace and regular exercises to strengthen the ankle.
If you have any questions please feel free to contact one of our offices located in Holmdel and Middletown, NJ . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Diabetes affects millions of people every year. Blood vessels located all over the body are damaged due to diabetes—even the blood vessels of the feet. Neuropathy, or nerve damage, can result from slower blood flow in the legs and feet. In diabetic patients, neuropathy is very important to monitor, as diabetics are at risk for developing ulcers.
Always washing and thoroughly drying the feet are pertinent parts of diabetic foot care. There should be a focus on cleaning between the toes. Even if no pain is felt, the entire foot should be examined for redness and sores. Neuropathy can often mask the pain of sores and ulcers and can cause these conditions to be overlooked. Use a mirror to examine the underside of your feet if needed. It is recommended that diabetics wear well-fitting socks.
Patients with diabetes should have their doctor monitor their blood levels because blood sugar levels play a huge role in diabetic care. Monitoring these levels on a regular basis is highly advised. It is very important to keep your blood sugar levels in the normal range, which can be determined by your physician. There are medications that may be prescribed to help with any neuropathy experienced by the diabetic patient. It is also advisable to visit a podiatrist if one is experiencing any conditions involving the feet, such as ingrown toenails, which in more severe cases can cause infection.
Diabetic feet must be inspected daily. Diabetic foot care at home is possible if a patient is provided with instructions from their podiatrist. Patients can relieve dry heels with creams or ointments. Suspected wounds should warrant an immediate call to the podiatrist. Gangrene is a serious problem for diabetics and can lead to sepsis and amputation in its worst cases. Early treatment and daily inspection of diabetic feet are keys to staying healthy.
 Diabetes is a systemic condition that can affect many parts of your body – including the feet. Due to the chronically raised blood sugar levels associated with diabetes, the nerves and blood vessels that supply the lower limbs can become damaged. This can cause neuropathy and poor circulation, both of which can lead to strange sensations, such as burning and tingling or numbness in the feet, a loss of sensation, and the formation of poorly healing foot wounds. The skin and nails on the feet may also change. Skin can become dry and cracked, and start to peel, and calluses may form more quickly, as well. Because diabetes can also cause immune insufficiency, foot and nail infections are more likely to occur. If you have diabetes, it is suggested that you visit a podiatrist regularly to monitor and preserve the health of your feet.
Diabetes is a systemic condition that can affect many parts of your body – including the feet. Due to the chronically raised blood sugar levels associated with diabetes, the nerves and blood vessels that supply the lower limbs can become damaged. This can cause neuropathy and poor circulation, both of which can lead to strange sensations, such as burning and tingling or numbness in the feet, a loss of sensation, and the formation of poorly healing foot wounds. The skin and nails on the feet may also change. Skin can become dry and cracked, and start to peel, and calluses may form more quickly, as well. Because diabetes can also cause immune insufficiency, foot and nail infections are more likely to occur. If you have diabetes, it is suggested that you visit a podiatrist regularly to monitor and preserve the health of your feet.
Diabetic foot care is important in preventing foot ailments such as ulcers. If you are suffering from diabetes or have any other concerns about your feet, contact one of our podiatrists from Biebel & DeCotiis Podiatry Associates. Our doctors can provide the care you need to keep you pain-free and on your feet.
Diabetic Foot Care
Diabetes affects millions of people every year. The condition can damage blood vessels in many parts of the body, especially the feet. Because of this, taking care of your feet is essential if you have diabetes, and having a podiatrist help monitor your foot health is highly recommended.
The Importance of Caring for Your Feet
- Routinely inspect your feet for bruises or sores.
- Wear socks that fit your feet comfortably.
- Wear comfortable shoes that provide adequate support.
Patients with diabetes should have their doctor monitor their blood levels, as blood sugar levels play such a huge role in diabetic care. Monitoring these levels on a regular basis is highly advised.
It is always best to inform your healthcare professional of any concerns you may have regarding your feet, especially for diabetic patients. Early treatment and routine foot examinations are keys to maintaining proper health, especially because severe complications can arise if proper treatment is not applied.
If you have any questions please feel free to contact one of our offices located in Holmdel and Middletown, NJ . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Broken Feet
A broken foot can either refer to a fracture or a straight break. The location of any break can tell you how the break happened. Toes, for instance, break typically as a result of something being kicked hard and with great force. Heel breaks almost always are a result of an improper landing from a tall height. Twists or sprains are the other two frequent occurrences. As with all usual breaks, they result from unexpected accident or sudden injury. As with stress fractures, breaks form as a process over time from repeated stress on already present cracks. Runners, dancers, and gymnasts are the usual athletes who receive this type of break. Stress fractures result from incredible pressure on the feet. It is no surprise these athletes bear the majority of reported fractures.
Pain, swelling, bruising, and redness are all indicative of the typical symptoms from a broken foot. Severe pain—to the point of not being able to walk—usually depends on the location of the break in the foot. Toes are on the lower scale of pain threshold, but heels are high, as are a few other particular bones. As the severity of the broken foot increases, symptoms like blueness, numbness, misshaping of the foot, cuts, or deformities will become apparent. These symptoms indicate the need to see a medical professional with access to an x-ray facility.
Prior to seeing a specialist, precautions should be taken to reduce pain and swelling. Elevate and stabilize the foot, and refrain from moving it. Immobilization of the foot is the next priority, so creating a homemade splint is acceptable. Keep in mind that while creating a splint, any increase of pain or cutting off blood circulation means that the splint should be removed immediately. Use ice to decrease swelling and relieve pain symptoms.
When dealing with a medical center, the patient should note that the treatment can vary. The treatment will depend on the severity of the fracture and the cause of the break. Crutches, splits, or casts are common treatments while surgery has been known to be used in more severe cases in order to repair the break in the bones.
Broken Ankles
Broken ankles are a serious injury that can lead to an inability to walk, function, and also cause a significant amount of pain. A broken ankle is a break in one of the three bones in your body that connect at the ankle joint, the tibia, the fibula, and the talus. The tibia and fibula are your two primary leg bones that connect at the knee, which sits directly upon the talus bone. This is protected by a fibrous membrane that allows for movement in our ankle joint. A broken ankle is usually caused by the foot rolling under or twisting too far, causing one of these three bones to snap.
A broken ankle is different from an ankle sprain, which occurs when the ligaments are ripped or torn but no bones have been broken. A sprain can still be very severe, causing bruising in the foot and an inability to hold your own weight, much like a broken ankle would. If you’re unable to stand, and suspect that you have a broken ankle, the first thing to do would be to get an immediate x-ray to determine the severity of the break.
A common cause of broken ankles is when the ankle is rolled over with enough pressure to break the bones. This usually happens during exercise, sports, or other physical activities. Another common cause is a fall or jump from a tall height.
One immediate treatment for pain relief is elevating the feet above your head to reduce blood flow to the injured area. You can also apply ice packs to your ankles to help reduce swelling, redness, inflammation, and pain. After these initial steps, getting a cast and staying off your feet as much as possible will aid in the recovery of the broken ankle. The less movement and stress the ankle has to endure, the more complete it will heal. A doctor can determine if surgery is needed in order to heal correctly. In these cases, an operation may be the only option to ensure the ability to walk properly again, followed by physical therapy and rehabilitation.
It is highly important to determine if surgery is needed early on, because a broken ankle can become much more severe than you realize. If not professionally treated, the broken ankle will inhibit your walking, daily functioning, and produce a large amount of pain. Treating your broken ankle early on will help prevent further damage to it.
 If you are experiencing severe pain and swelling in the midfoot area and are having trouble bearing weight on your foot, you may have sustained a Lisfranc joint injury. This joint is a band of tissue that connects the long bones that lead to the toes to the tarsal bones in the arch and helps with alignment and strength of the foot. Bruising and an unusual widening of the foot are other signs of a problem. Injuries to this joint may occur directly, by dropping something heavy on your foot, or indirectly like the result from twisting your foot. It is most common in runners, athletes who play contact sports, and victims of car accidents. It can also be caused by something as simple as tripping on the stairs. In such injuries a ligament may be torn or stretched, or a bone may be fractured or dislocated. If your symptoms become worse, it’s a good idea to contact a podiatrist as quickly as possible for a full examination to determine a treatment plan. In the meantime it is suggested that you stay off the injured foot, wrap it to keep the swelling down, apply ice to the area, and keep it elevated when sitting or lying down.
If you are experiencing severe pain and swelling in the midfoot area and are having trouble bearing weight on your foot, you may have sustained a Lisfranc joint injury. This joint is a band of tissue that connects the long bones that lead to the toes to the tarsal bones in the arch and helps with alignment and strength of the foot. Bruising and an unusual widening of the foot are other signs of a problem. Injuries to this joint may occur directly, by dropping something heavy on your foot, or indirectly like the result from twisting your foot. It is most common in runners, athletes who play contact sports, and victims of car accidents. It can also be caused by something as simple as tripping on the stairs. In such injuries a ligament may be torn or stretched, or a bone may be fractured or dislocated. If your symptoms become worse, it’s a good idea to contact a podiatrist as quickly as possible for a full examination to determine a treatment plan. In the meantime it is suggested that you stay off the injured foot, wrap it to keep the swelling down, apply ice to the area, and keep it elevated when sitting or lying down.
Foot and ankle trauma is common among athletes and the elderly. If you have concerns that you may have experienced trauma to the foot and ankle, consult with one of our podiatrists from Biebel & DeCotiis Podiatry Associates. Our doctors will assess your condition and provide you with quality foot and ankle treatment.
Foot and ankle trauma cover a range of injuries all over the foot; common injuries include:
- Broken bones
- Muscle strains
- Injuries to the tendons and ligaments
- Stress fractures
Symptoms
Symptoms of foot and ankle injuries vary depending on the injury, but more common ones include:
- Bruising
- Inflammation/ Swelling
- Pain
Diagnosis
To properly diagnose the exact type of injury, podiatrists will conduct a number of different tests. Some of these include sensation and visual tests, X-rays, and MRIs. Medical and family histories will also be taken into account.
Treatment
Once the injury has been diagnosed, the podiatrist can than offer the best treatment options for you. In less severe cases, rest and keeping pressure off the foot may be all that’s necessary. Orthotics, such as a specially made shoes, or immobilization devices, like splints or casts, may be deemed necessary. Finally, if the injury is severe enough, surgery may be necessary.
If you have any questions, please feel free to contact one of our offices located in Holmdel and Middletown, NJ . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Peripheral artery disease (PAD), or peripheral arterial disease, is a circulatory problem in which there is a reduction of blood flow to the limbs due to narrowed arteries. When peripheral artery disease develops, the extremities do not receive enough blood flow; this may cause symptoms to develop such as claudication, or leg pain when walking. The legs are the most common site of peripheral artery disease.
Claudication, or leg pain when walking, is one of several symptoms that can develop due to peripheral artery disease. Other symptoms caused by the disease include painful cramping in the hips, thighs, or calves after certain activities; leg numbness or weakness; coldness in the lower leg or foot; sores on the lower extremities that do not heal; hair loss on the lower extremities; and a missing or weak pulse in the lower extremities. In more severe cases, pain may even occur when the body is at rest or when lying down.
Peripheral artery disease is typically caused by atherosclerosis, a condition in which fatty deposits build up in the arterial walls and reduce blood flow. Smoking, diabetes, obesity, high blood pressure, and high cholesterol are some of the risk factors for peripheral artery disease.
If you are experiencing pain, numbness, or other symptoms in the lower extremities, see your healthcare professional immediately. Diagnosed peripheral artery disease can be treated with various medications, angioplasty and surgery, exercise programs, or alternative medicine. It is important to consult a healthcare professional to determine the best treatment for you.